About This Article: Zoom Health has supplied home health tests to UK customers for nearly 20 years. This guide draws on our experience helping thousands of people monitor their health and understand Type 1 diabetes. Always consult a healthcare professional for medical advice.
Table of Contents
- What Is Type 1 Diabetes?
- Type 1 vs Type 2 Diabetes: Key Differences
- Recognising Type 1 Diabetes Symptoms
- Living With Type 1 Diabetes
- Diet and Meal Planning
- Checking Blood Sugar Levels
- Insulin Therapy Basics
- Dealing With High and Low Blood Sugar
- Reducing Risk of Complications
- Home Testing for Diabetes
- Frequently Asked Questions
What Is Type 1 Diabetes?
Type 1 diabetes is a chronic autoimmune condition affecting how the body produces insulin. The immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas, leaving the body unable to regulate blood sugar effectively. Without adequate insulin, glucose builds up in the bloodstream and can reach dangerously high levels.
Type 1 diabetes is most commonly diagnosed in children and adolescents, though it can develop in adults at any age. In the UK, more than 400,000 people have Type 1 diabetes, with around 29,000 new diagnoses each year. Unlike Type 2 diabetes, it is not caused by diet or lifestyle choices—it’s primarily genetic.
Since the body cannot produce its own insulin, people with Type 1 diabetes must take insulin via injections or an external pump to survive. With proper management including regular monitoring, insulin therapy, and lifestyle adjustments, most people with Type 1 diabetes live long, active, healthy lives.
Key Point: Type 1 diabetes is not preventable and has no cure—but it is very manageable with the right knowledge, support, and monitoring tools.
Type 1 vs Type 2 Diabetes: Key Differences
While both affect blood sugar control, Type 1 and Type 2 diabetes are distinct conditions. Type 1 is an autoimmune condition where the pancreas stops producing insulin altogether. Type 2, which accounts for around 90% of diabetes cases, occurs when the body becomes resistant to insulin or the pancreas doesn’t produce enough—and it’s strongly linked to lifestyle factors like diet and weight.
Quick Comparison
- Type 1: Autoimmune; pancreas produces little or no insulin; usually diagnosed in children/young adults; requires lifelong insulin therapy
- Type 2: Insulin resistance; pancreas produces some insulin; usually diagnosed in adults; often managed through diet, exercise, and medication (though insulin may be needed later)
- Causes: Type 1 is genetic; Type 2 is linked to genetics, weight, lifestyle, and age
- Prevention: Type 1 cannot be prevented; Type 2 can often be prevented or delayed through lifestyle changes
Recognising Type 1 Diabetes Symptoms
Type 1 diabetes symptoms often develop quickly—sometimes over just a few weeks. Recognising these early signs is important for seeking prompt medical attention. According to NHS guidance, common Type 1 diabetes symptoms include:
- Frequent urination, especially at night
- Excessive thirst and dry mouth
- Unusual weight loss despite increased appetite
- Extreme fatigue or tiredness
- Blurred vision
- Irritability or mood changes
- Slow healing of cuts or wounds
- Fruity-smelling breath (in severe cases)
If you or someone you know experiences any of these symptoms, see a doctor right away. Early diagnosis is crucial to prevent serious complications like diabetic ketoacidosis (DKA), a life-threatening condition.
Living With Type 1 Diabetes
A Type 1 diabetes diagnosis can feel overwhelming. However, with the right knowledge, tools, and support, most people manage it effectively and live full, active lives. According to NICE (National Institute for Health and Care Excellence) guidance on Type 1 diabetes management, successful management requires a combination of insulin therapy, regular blood sugar monitoring, healthy eating, and physical activity.
Diet and Meal Planning
There’s no strict “diabetes diet,” but eating a balanced, nutritious diet is essential. Work with a registered dietitian or diabetes educator to create a personalised meal plan that fits your lifestyle and blood sugar targets.
Key Dietary Principles for Type 1 Diabetes
- Monitor carbohydrates: Carbohydrates have the biggest impact on blood sugar levels. Track portions and aim for consistency at each meal.
- Choose whole foods: Eat plenty of vegetables, fruits, whole grains, lean proteins, and healthy fats (olive oil, avocados, nuts).
- Stay hydrated: Drink water or low/no-calorie beverages. Avoid sugary drinks.
- Meal timing: Eat meals and snacks at consistent times to match your insulin doses.
- Professional guidance: A registered dietitian can help you understand how specific foods affect your blood sugar and insulin needs.
Checking Blood Sugar Levels
Regular blood sugar monitoring is essential for managing Type 1 diabetes effectively. A finger prick test using a glucose meter measures the amount of glucose in your blood at any given moment.
- Test when waking up, before meals, 1–2 hours after meals, before bedtime, and whenever you suspect low or high blood sugar
- Keep a logbook or use a digital app to track results—this helps identify patterns and guides treatment decisions
- Work with your medical team to set personal blood sugar targets (typical targets: 80–130 mg/dL before meals, under 180 mg/dL after meals)
- Aim for an HbA1c level below 7% to reduce the risk of long-term complications
What Customers Say
★★★★★ Mark W. – October 2022
“Bought it to test me and the wife for diabetes, but it tests for lots of other parameters too. Found out I am quite badly dehydrated and the wife is moderately dehydrated. No sign of diabetes.”
★★★★★ Lorraine H. – June 2025
“The diabetes test kit was simple to do and fast, it also put my mind at ease. A good all rounder.”
★★★★★ Prof Eddie Fisher – April 2023
“Easy to use and follow test instructions including a well laid-out test result table.”
Insulin Therapy Basics
Since people with Type 1 diabetes cannot produce their own insulin, insulin therapy is essential and must be taken daily, often multiple times per day.
Understanding Insulin Therapy
- Delivery methods: Multiple Daily Injections (MDI) or an insulin pump—choose the method that best fits your lifestyle
- Types of insulin: Different insulins work at different speeds and durations. Your doctor may prescribe a combination to mimic natural insulin responses
- Dose adjustment: Insulin needs vary based on food intake, activity level, stress, illness, and hormonal changes. Expect regular adjustments with guidance from your healthcare team
- Hypoglycaemia risk: Taking insulin increases the risk of low blood sugar. Always carry fast-acting carbohydrates (e.g. glucose tablets, sweets) and have an emergency glucagon kit available
Dealing With High and Low Blood Sugar
Managing blood sugar involves recognising and treating both high (hyperglycaemia) and low (hypoglycaemia) blood sugar episodes.
Low Blood Sugar (Hypoglycaemia)
Symptoms: shakiness, sweating, anxiety, hunger, confusion, irritability. Treatment: Consume 15–20g of fast-acting carbohydrates (glucose tablets, juice, or sweets). Recheck after 15 minutes. If symptoms persist, treat again. Always have emergency glucagon available, and teach family/friends how to administer it.
High Blood Sugar (Hyperglycaemia)
Symptoms: excessive thirst, frequent urination, fatigue, blurred vision. Treatment: Take insulin as directed by your healthcare team. Drink plenty of water. If accompanied by nausea, vomiting, or fruity-smelling breath, seek emergency medical help (diabetic ketoacidosis).
Exercise and hypoglycaemia: Physical activity lowers blood sugar. Check levels before, during, and after exercise. Adjust insulin doses and carbohydrate intake according to your activity level to prevent low blood sugar episodes.
Reducing Risk of Complications
Long-term complications of Type 1 diabetes include heart disease, kidney damage, nerve damage, and eye problems. The good news: maintaining good blood sugar control significantly reduces these risks.
Key Steps to Prevent Complications
- Control blood sugar: Keep HbA1c below 7% to significantly reduce risk of kidney, nerve, and eye damage
- Eye health: Get a dilated eye exam yearly to screen for diabetic retinopathy. Early detection prevents vision loss
- Heart and kidney health: Monitor blood pressure and cholesterol. Manage through diet, exercise, and medication if needed. The British Heart Foundation offers resources on cardiovascular health for people with diabetes
- Foot care: Inspect feet daily for cuts, blisters, or irritation. Seek prompt treatment to prevent infections. See a podiatrist regularly if needed
- Kidney screening: Have regular kidney function tests and urine checks to catch early kidney disease
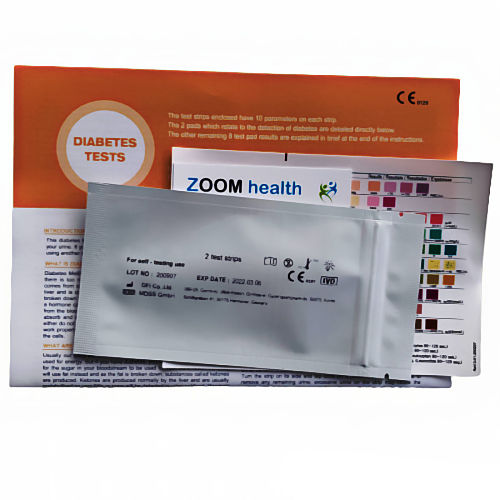
Home Testing for Diabetes
If you suspect you might have diabetes or want to check your urinary glucose and ketone levels, a home diabetes test kit can provide initial screening results. Our home diabetes test kit measures both glucose and ketones in urine, helping identify diabetes at an early stage before symptoms develop. Results appear in just 60 seconds.
Important note: Home urine tests are screening tools, not diagnostic. A positive result should always be confirmed with a blood test from your GP. Only blood tests can definitively diagnose diabetes.
If you suspect Type 1 diabetes: Seek medical attention promptly. Home tests can help, but a doctor must perform blood tests (fasting glucose, random glucose, or HbA1c) to confirm diagnosis.
Frequently Asked Questions
Can Type 1 diabetes be prevented?
No, Type 1 diabetes cannot be prevented. It’s an autoimmune condition with a strong genetic component. Lifestyle changes cannot prevent it, though maintaining a healthy lifestyle after diagnosis helps with management.
Can you live a normal life with Type 1 diabetes?
Yes, absolutely. With proper insulin management, regular blood sugar monitoring, and a healthy lifestyle, most people with Type 1 diabetes live long, active, fulfilling lives. Many professional athletes, doctors, and successful individuals manage Type 1 diabetes daily.
Is there a cure for Type 1 diabetes?
Currently, there is no cure for Type 1 diabetes. However, research is ongoing into potential treatments including pancreas transplants, artificial pancreases, and immunotherapy approaches. In the meantime, insulin therapy and modern diabetes management tools enable excellent health outcomes.
How often should I check my blood sugar?
Most people with Type 1 diabetes test at least 4–8 times daily: when waking, before meals, after meals, and before bed. Your doctor may recommend more frequent testing during illness, exercise, or periods of unstable blood sugar. Continuous glucose monitors (CGMs) track levels automatically throughout the day.
Can people with Type 1 diabetes eat sugar?
People with Type 1 diabetes can eat foods with sugar, but portion control and carbohydrate counting are essential. The key is matching insulin doses to carbohydrate intake. Work with a dietitian to learn how to balance treats within your overall meal plan.
What is HbA1c and why does it matter?
HbA1c (glycated haemoglobin) is a blood test measuring average blood sugar control over the past 2–3 months. It’s more useful than single daily readings for assessing long-term management. An HbA1c below 7% (53 mmol/mol) is the typical target for people with Type 1 diabetes and significantly reduces complication risks.
About the Author
Anthony Cunningham – Health Writer & Editor
Anthony Cunningham, BA (Hons), MA, is a UK-based health writer and editor with over 20 years’ experience running Zoom Health, a trusted source for home health tests, preventive care, and wellness guidance. He creates clear, evidence-based articles using NHS, NICE, and WHO guidance. Where possible, content is reviewed by practising clinicians to enhance accuracy and reliability, helping readers make informed healthcare decisions.
Originally published: 2023 | Last updated: November 13, 2025